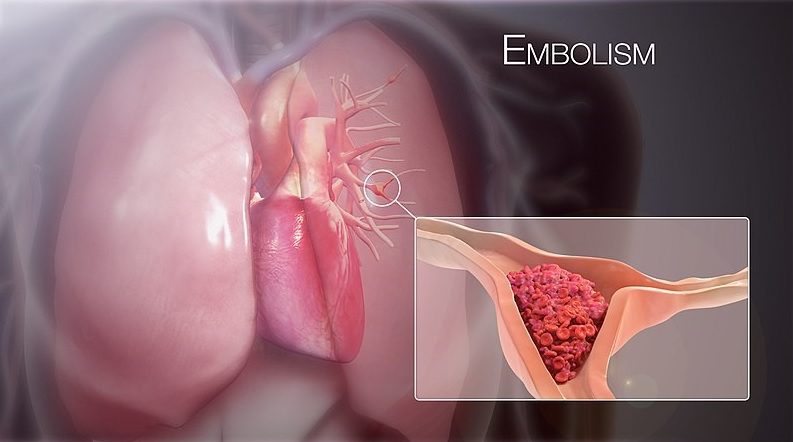
IntrPulmonary Embolism
Pulmonary embolism is a clinical condition arising due to the presence of a clot (Thrombus) within the pulmonary artery or its branches causing obstruction to the flow of the blood. Mostly, these clothes originated within the deep veins of the lower extremities which later dislodges and enter pulmonary arteries. Sometimes, other materials like air, fat, or tumor cells can also enter into the pulmonary circulation causing obstruction to the blood flow. [1]
It is the third most common type of cardiovascular disease after coronary artery disease and stroke, affecting males more than females with an incidence of (39-115) per 100,000 population [2] with a mortality rate of 100,000/year in the US. [3]
IntrPulmonary Embolism
The risk factors for the thrombus to develop within the deep veins can be explained by Virchow’s Triad: Hypercoagulability, venous stasis, and endothelial injury. [4]
Hypercoagulability:
- Factor V Leiden mutation.
- Prothrombin gene mutation.
- Protein C deficiency.
- Protein S deficiency.
- Homocystinuria.
- Oral Contraceptives.
- Hormone replacement therapy.
Venous Stasis:
- Bedridden/Bed rest status (>3days).
- Traveling status (>4hours).
- Recent orthopedic surgery, fractures of the lower limb, major trauma.
- Malignancy.
- Obesity.
- Pregnancy.
- Heart failure, Atrial Fibrillation.
- Postpartum period.
Endothelial injury:
- Indwelling venous catheter.
- Cigarette smoking.
- Orthopedic surgeries, Hip/Knee replacement surgeries.
- Radiation.
Others:
Cancers (Pancreatic, Hematologic, Lung, Gastric, Brain Cancers)
Pathophysiology
Pulmonary embolism starts as a result of the breakage of clots from the deep veins thrombosis of lower limbs. Most of the time, the emboli are typically multiple in number and affect the lower lobes of bilateral lungs. If the emboli are large, it gets trapped within the main pulmonary artery (saddle emboli) and can cause serious cardiovascular insufficiency (Hypotension). Smaller emboli block peripheral arteries and can lead to infarction of the lobe causing intra-alveolar hemorrhage.
Any type of emboli leads to inadequate gas exchange (mismatch in ventilation-perfusion ratio), alterations in lung surfactant, respiratory drive stimulation, and ultimately resulting in Hypocapnia and respiratory alkalosis.
Larger emboli occluding 30% to 50% of the cross-sectional area of the pulmonary artery increases right ventricular afterload causing dilatation. Left ventricular filling is consequently reduced, causing systemic hypotension and hemodynamic instability. Acute pressure overload in the right ventricle causing right ventricular failure is the primary cause of mortality in severe pulmonary embolism.
Types
Based on the presence of hemodynamic instability, PE can be sub-categorized as:
- Hemodynamically Unstable PE (massive/high-risk PE): Pulmonary embolism associated with hypotension (systolic BP <90mmHg, or drop in systolic BP of 40mmHg or more from baseline; requiring Inotropes). It is associated with a higher rate of mortality due to obstructive shock/severe right ventricular failure.
- Hemodynamically stable PE (sub-massive/ Intermediate risk PE):
Patients in this category have mild Hypotension which responds to fluid therapy or have right ventricular dysfunction only. Some patients even might be asymptomatic (low-risk PE/ Small PE).
Diagnosis
Symptoms:
Dyspnea- acute, severe in central and mild and transient in small, peripheral PE.
Pleuritic chest pain: in distal emboli.
- Cough.
- Hemoptysis.
- Syncope.
- Atrial fibrillations (less common).
- Careful workup for risk factors of deep venous thrombosis should be sought.
Signs:
- Tachycardia.
- Tachyp noea.
- Rales and decreased breath sounds.
- Signs of pulmonary hypertension: Jugular venous distension, loud P2 component in second Heart Sound.
- Right-sided gallop rhythm.
- Right p arasternal lift.
- Signs of massive emboli (indicative of acute ventricular failure): Jugular vein distension.
- Parasternal lift.
- 3rd heart sound.
- Cyanosis.
- Shock.
Sudden bradycardia in a patient with Tachycardia, new-onset complex Tachycardia, Right Bundle Branch Block indicates signs of severe right ventricular strain. [5]
Clinical prediction: [4]
- Revised Geneva Clinical Prediction Rule.
- Wells criteria and modified wells criteria.
- PERC rule.
Investigations:
- Chest X-ray: may be normal or may present atelectasis, effusion, or rare but specific signs like Hampton’s Hump, Westermark’s sign.
- Arterial Blood Gas Analysis: Unexplained Hypoxemia, Respiratory Alkalosis, Hypocapnia.
- (Massive PE can also present as Hypercapnia, respiratory or lactic acidosis).
- BNP (Brain Natriuretic Peptide): indicates severe right ventricular pressure overload.
- Troponin T and I: Although there is no diagnostic significance, the elevation of Troponins signifies right ventricular dysfunction, clinical deterioration and is linked with death.
- D-Dimer: Normal D-Dimer level makes acute PE/DVT less likely but elevated D-Dimer cannot confirm PE due to its low positive predictive value.
- ECG: Common ECG findings are Tachycardia, non-specific ST-segment, and T-wave changes with S1Q3T3 pattern, right ventricular strain, Right Bundle Branch Block. These findings are, however, non-specific.
- Computed Tomographic Pulmonary Angiography (CTPA): CTPA is the investigation modality of choice. It has a high positive predictive value (92%-96%). It can detect PE along with right ventricular enlargement.
- Lung Scintigraphy (Ventilation-Perfusion scan (V/Q scan)): It is an established diagnostic test but is mostly performed when CTPA is inconclusive/contraindicated. It is an investigation of choice for the diagnosis of PE in pregnancy.
Pulmonary Angiography
In the past, Pulmonary Angiography was the gold standard testing modality for PE. The test is still performed when CTPA and V/Q scanning is contraindicated or is inconclusive.
Treatment
- Management of acute cases.
- Supportive measures:
- Supplemental oxygen when oxygen saturation is <90%.
- Mechanical ventilation in unstable patients
- Volume resuscitation (tried only in collapsible IVC/Intravascular volume depletion).
- Vasopressors.
- Extracorporeal membrane Oxygenation (ECMO) devices for mechanical cardiopulmonary support may be used in unstable patients.
- Anti-coagulation: started even before diagnostic images are available in the patients with high suspicion for PE.
- The mainstay of treatment in acute PE.
- Low-Molecular-Weight Heparin (LMWH) or Fondaparinux (preferred) or Unfractionated Heparin.
- Unfractionated Heparin is used only when there is Hemodynamic Instability and patients might need primary reperfusion treatment or have renal dysfunction.
Reperfusion therapies [4]:
- Thrombolysis:
Reperfusion with thrombolysis provides the greatest mortality benefit when started early (within 48hours of onset of symptoms). Improvement can be assessed by a decrease in right ventricular dilatation on Echocardiography.
However, due to the increased risk of bleeding, these therapies are contraindicated in:
- Any prior intracranial hemorrhage.
- Ischemic stroke within 3 months.
- Suspected Aortic Dissection.
- Active bleeding/ bleeding diathesis.
- Recent cranial/ GI surgeries.
- Recent Head/Facial trauma.
- Catheter guided treatment:
In this treatment method, a catheter is inserted or ascended up to the pulmonary arteries, and then it is used for thrombolysis (ultrasound-guided or pharmacological means combined with mechanical fragmentation), suction, aspiration, or embolectomy. The success rate is high (up to 87%) but carries a risk of perforation of pulmonary arteries, and can rarely lead to massive hemoptysis or cardiac tamponade. Newer technologies like FlowTriever System are found to be safe and effective method for removal of the thrombus. [6]
- Surgical Embolectomy: surgical removal of embolus is performed when a hemodynamically Unstable patient has contraindications to or does not respond to thrombolysis. Studies indicate that there is no difference in mortality between the two.
- Vena cava filters: The filters are placed in Inferior Vena Cava to block the emboli from ascending to the right heart and subsequently to the pulmonary arteries. The filters are mainly indicated in recurrent venous thromboembolism despite adequate anticoagulation and when there are absolute contraindications to anticoagulants. The filters are discontinued once the anticoagulants can be safely used in the patients. These devices although decrease the risk of recurrent PE, can increase the risk of DVT.
B. Treatment in Chronic cases/ prevention of recurrence:
All patients should receive 3 months or more of anticoagulation therapy. However, after discontinuation, the risk of recurrence is similar and oral anticoagulants can be used thereafter. Oral anticoagulants can be used for extended periods if PE is unprovoked (PE occurring without risk factors) or if there are persistent risk factors for thrombus formation.
References:
- Coon WW, Willis III PW. Deep venous thrombosis and pulmonary embolism: Prediction, prevention and treatment∗. The American journal of cardiology. 1959 Nov 1;4(5):611-21.
- Wendelboe AM, Raskob GE. Global Burden of Thrombosis: Epidemiologic Aspects. Circ Res. 2016 Apr 29;118(9):1340-7.
- Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States, 1979-1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003 Jul 28;163(14):1711-7.
- Vyas V, Goyal A. Acute pulmonary embolism. StatPearls [Internet]. 2020 Aug 10.
- Kucher N, Goldhaber SZ. Management of massive pulmonary embolism. Circulation. 2005 Jul 12;112(2):e28-32.
- https://advances.massgeneral.org/cardiovascular/journal.aspx?id=1360