Congestive heart failure occurs when the heart muscle does not pump blood as well as it should. Certain pathologies, such as narrowed arteries in the heart (coronary artery disease) or high blood pressure, leave the heart progressively too weak or rigid to fill and pump effectively.
It is not possible to reverse all the conditions that cause heart failure, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes (such as exercising, reducing sodium in the diet, managing stress and losing weight) can improve the quality of life.
Heart Failure symptoms
Heart failure may be constant (chronic) or may begin suddenly (acute).
Some of the signs and symptoms of heart failure may be the following:
- Shortness of breath (dyspnea) when you strain or lie down.
- Fatigue and weakness.
- Swelling (edema) in the legs, ankles and feet.
- Fast or irregular heartbeats.
- Less ability to exercise.
- Constant coughing or wheezing with white or pink blood-stained phlegm.
- Increased need to urinate at night.
- Edema of the abdomen (ascites).
- Very rapid weight gain due to fluid retention.
- Lack of appetite and nausea.
- Difficulty concentrating or less alertness.
- Chest pain if heart failure is the result of a heart attack.
Causes
Heart failure usually manifests after other conditions have damaged or weakened the heart. However, it is not necessary for the heart to be weakened to cause heart failure. This can also happen if the heart becomes too stiff.
In the case of heart failure, the main pumping cavities of the heart (the ventricles) can become stiff and not fill properly between beats. In other cases of heart failure, the heart muscle may weaken, and the ventricles stretch (dilate) to such an extent that the heart cannot pump blood throughout the body effectively.
Over time, the heart can no longer maintain the normal demands of pumping blood to the rest of the body.
An ejection fraction is an important measure of how well the heart pumps blood, and is used to help classify heart failure and to guide treatment. In a healthy heart, the ejection fraction is 50 percent or greater, which means that more than half of the blood that fills the ventricle is pumped out with each beat.
Heart failure can affect the left side (left ventricle), the right side (right ventricle) or both sides of the heart. Usually, heart failure begins on the left side, specifically, in the left ventricle (the main pumping cavity of the heart).
- Left heart failure, fluid can accumulate in the lungs, which will cause you to lack air.
- Right heart failure, fluid may accumulate in the abdomen, legs and feet, which will cause swelling.
- Systolic heart failure, the left ventricle cannot contract vigorously, indicating a pumping problem.
Diastolic heart failure (also called “heart failure with preserved ejection fraction”, the left ventricle cannot relax or fill completely, indicating a filling problem.
The following conditions can damage or weaken the heart and cause heart failure.
- Coronary artery disease and heart attack: Coronary artery disease is the most common form of heart disease and the most frequent cause of heart failure. The disease is due to an accumulation of fatty deposits (plaques) in the arteries, which reduces blood flow and can cause a heart attack.
- High blood pressure (hypertension): If the blood pressure is high, the heart has to work harder than it should to circulate blood through the body. Over time, this extra effort can cause the heart muscle to become too stiff or too weak to pump blood effectively.
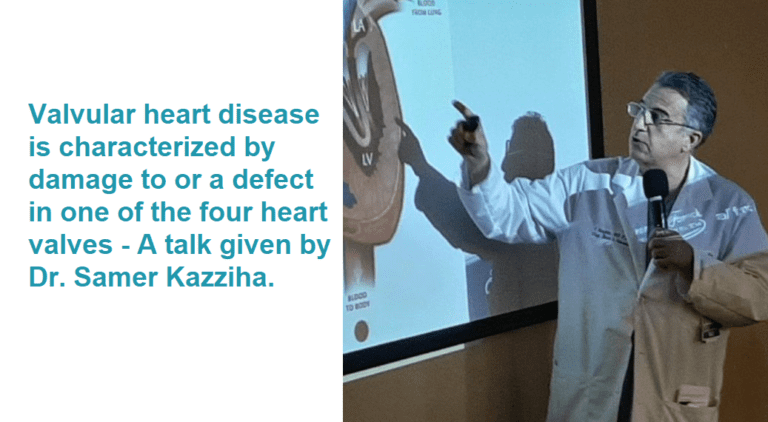
- Defective heart valves: Heart valves keep blood flowing in the right direction through the heart. A damaged valve (due to a heart defect, coronary artery disease or heart infection) forces the heart to work harder, which can weaken it over time.
- Damage to the heart muscle (cardiomyopathy): Damage to the heart muscle (cardiomyopathy) can have many causes, such as various diseases, infections, alcohol abuse and the toxic effect of drugs, such as cocaine, or some medications used in chemotherapy. Genetic factors could also influence.
- Myocarditis: Myocarditis is inflammation of the heart muscle. Its most frequent cause is a virus, and it can cause left heart failure.
- Birth cardiac defects (congenital heart defects). If the heart and its cavities or valves have not formed properly, healthy parts of the heart have to work harder to pump blood through the heart.
- Abnormal heart rhythms (cardiac arrhythmias). Abnormal heart rhythms can cause the heart to beat too fast, which creates additional effort. A slow heartbeat can also cause heart failure.
- Other diseases.: Chronic diseases such as diabetes, HIV, hyperthyroidism, hypothyroidism or an accumulation of iron (hemochromatosis) or protein (amyloidosis) can also contribute to heart failure.
Risk factors
A single risk factor may be sufficient to cause heart failure; However, a combination of factors increases the risk.
The risk factors are as follows:
- High blood pressure: The heart tries harder than it should if the blood pressure is high.
- Coronary artery disease: Narrowed arteries can limit the supply of oxygen-rich blood to the heart, which causes the heart muscle to weaken.
- Heart attack: A heart attack is a form of coronary heart disease that occurs suddenly. Damage to the heart muscle from a heart attack can mean that the heart can no longer pump in the right way.
- Diabetes: Having diabetes increases the risk of having high blood pressure and coronary artery disease.
- Some diabetes medications: It has been found that medications for diabetes rosiglitazone and pioglitazone increase the risk of heart failure in some people.
- Sleep apnea: The inability to breathe properly while you sleep at night generates low blood oxygen levels, and an increased risk of having abnormal heart rhythms. Both problems can weaken the heart.
- Congenital heart defects. Some people who manifest heart failure have been born with structural heart defects.
- Valvulopathy. People with valvulopathy are at greater risk for heart failure.
- Virus: A viral infection may have damaged the heart muscle.
- Alcohol consumption. Drinking too much alcohol can weaken the heart muscle and cause heart failure.
- Tobacco use. The use of tobacco may increase the risk of heart failure.
- Obesity: Obese people are at greater risk of heart failure.
Complications.
The prognosis depends on the cause, severity and age. Complications can be the following:
• Damage or kidney failure. Heart failure can reduce blood flow to the kidneys, which can eventually lead to kidney failure if left untreated. Kidney damage due to heart failure may require dialysis as treatment.
• Heart valve problems. Heart valves, which maintain the flow of blood in the proper direction in this organ, may not work properly if the heart is dilated or if the pressure in the heart is very high due to heart failure.
• Heart rhythm problems. Heart rhythm problems (arrhythmias) can be a possible complication of heart failure.
• Hepatic injury. Heart failure can cause a buildup of fluid that puts too much pressure on the liver. This accumulation of fluid can cause scarring, which makes it more difficult for the liver to function properly.
The symptoms and cardiac function of some people will improve with proper treatment. However, heart failure can be life-threatening. People with heart failure may have severe symptoms, and some may require a heart transplant or help with a ventricular assist device.
Prevention.
The key to avoiding heart failure is to reduce risk factors. You can control or eliminate many of the risk factors for heart disease (such as high blood pressure and coronary artery disease) by implementing lifestyle changes along with the help of any necessary medication.
Lifestyle changes you can make to prevent heart failure include the following:
- No Smoking
- Control certain conditions, such as high blood pressure and diabetes
- Stay physically active
- Eat healthy foods
- Keep a healthy weight
- Reduce and control stress
Treatment of heart failure.
- Treat the cause that produces it (revascularization with angioplasty or bypass if it is due to lack of irrigation, stop drinking if you are an alcoholic).
- Control weight, low salt diet, control fluid intake, achieve normal weight.
- Diuretics improve congestive symptoms and reduce swelling or pulmonary congestion.
- Vasodilator drugs (such as nitrates or angiotensin-converting enzyme inhibitors and receptors) reduce the burden with which the heart must work, increase its performance and lower blood pressure. The latter are essential if the function of the heart is diminished.
- Beta blockers decrease pulsations and improve the prognosis (they are essential if the function of the heart is diminished).
- Digoxin is indicated in patients with atrial fibrillation.
- Aldosterone inhibitors are also necessary, as they improve survival in patients with diminished heart function.
- Ivabradine is a drug that exclusively reduces heart rate and may be beneficial in some types of heart failure.
- In other cases it is necessary to implant devices to patients who, despite a correct treatment (weight loss, proper diet, etc.), continue with symptoms, have certain ECG alterations and a decreased heart function (<35 %). These devices in patients with adequate life expectancy can improve symptoms or decrease the chance of dying suddenly.
- If the patient does not improve with all previous treatments, the cardiac transplant could be considered (depending on age and the presence of other diseases or complications).